Ravi Gupta
In the past 30 years, the number of patients suffering from osteoarthritis (OA) of various joints in India has risen threefold: from 2.3 crore in 1990 to 6.2 crore in 2019. Among these, knee remains the most affected joint, followed by OA of hand.
The ends of the bones constituting a joint are normally covered by a highly fine cartilage known as hyaline cartilage, which provides gliding surface to the bone end as well as a covering layer to the pain nerve endings in the bony tissue. In OA, this cartilage gets worn out, leading to exposure of coarse bony surfaces and exposing the pain fibres of the nerve endings in the bones, which cause pain. In response to the pain, inflammatory substances are secreted, causing a swollen joint. Thus, OA joints can present as painful swollen joints.
The usual predisposing factors of OA include advanced age, obesity, injuries and enhanced wear and tear in certain professions that require strenuous activities, causing injuries to the joint. Additionally, the malalignment of the lower limb bones, usually due to genetic predispositions, cause point loading on the joint surfaces, expediting the wear and tear of cartilage.
Based on X-rays, OA of the knee has been categorised into four grades, with Grade 1 being the mildest and Grade 4 the most severe. In the first three grades, no surgery is required and treatment includes strengthening of the thigh muscles, certain chondroprotective (cartilage protecting) drugs, reduction of body weight in obese individuals, and sometimes injections of lubricants or growth stimulating substances in the joints.
In advanced Grade 4 cases, the treatment is usually surgical. This surgery, known as joint replacement surgery, involves removing thin slices of the worn-out joint surfaces of constituent bones and covering the residual bone surfaces with artificial materials so that the pain nerve endings are not exposed. The most commonly used materials during this surgery are metallic surface on one side and a plastic-like material, polyethylene, on the other. These artificial surfaces of the joint, when subjected to the mechanical stresses of daily life, also get worn out with time, and ultimately, the patient may again start experiencing pain.
The average life of an artificial knee joint has been estimated to be around 15-20 years, which depends upon the activity level of the individual. The wear and tear is rapid in young, active persons as compared to elderly, inactive patients. Thus, the routine dictum is that the life of an artificial joint should last longer than the life of the patient, because the revision surgery of a worn-out artificial joint is more cumbersome and less successful as compared to the primary (or first) surgery. Therefore, the ideal age of a patient for undergoing such surgery should be beyond 65 years of age. In exceptional cases, when there’s severe crippling pain, the joint replacement can also be performed in younger patients with informed consent of the patient about the life of the artificial joint.
Probable risk factors
The risks and complications of knee replacement surgery are usually uncommon and can include infection, stiffness and loosening of the artificial joint surfaces, requiring more surgeries.
Patients can and should start walking using their knees immediately in the first couple of days after the surgery. The patients may need support of a walker or stick for the first four to six weeks. By around three months, the patients are quite comfortable walking. As a precautionary measure, these patients are usually advised to avoid squatting for the rest of their life due to the design of the artificial joints to enhance the longevity of the implant.
In the past four decades, many improvisations have been tried in the materials and design of the artificial joints with an aim to increase their average life. But as on today, most of the designs and materials have almost similar outcomes/lifespan.
In recent years, robotic replacement surgery has also become popular. The results, however, till today are inconclusive and there is no concrete evidence as to whether robotic surgery has superior results vis-a-vis traditional surgery.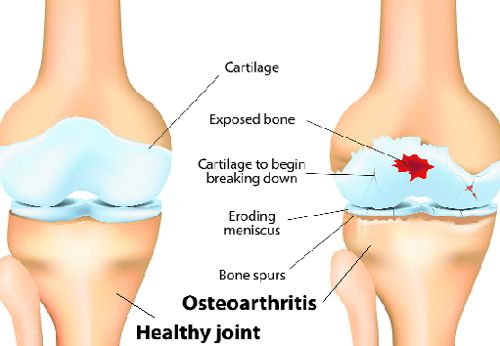
Cases where knee replacement surgery is recommended
- Severe longstanding pain restricting social life.
- The pain score between 0 and 10 being more than 6, where 0 means no pain and 10 means crippling pain, giving immobility.
- Patient’s age is more than 65 years.
- All non-operative treatment modalities, including weight reduction, muscle-strengthening exercises, physiotherapy and medical drugs have been already exhausted.
- The patient is medically fit to undergo this major surgery.
Possible pitfalls during/of surgery
- Infection during post-operative period.
- Stiffness of the joint.
- Residual pain.
- Clicks and clunks from the joint.
- Loosening of the artificial joint surfaces, causing painful joint.
- Deep vein thrombosis.
Precautions during recovery
- Exercises of various muscles of the knee and foot and an early out-of-bed mobility to keep the blood in circulation that prevents the complication of deep vein thrombosis.
- Proper intake of medications as advised.
- Optimum physiotherapy.
- Plenty of water intake in the post-operative period.
- No smoking.
- Intake of a high-protein diet.
Preventive measures
- Keep body weight in check.
- Moderate exercise, especially muscle-strengthening exercises of calf and thighs, and flexibility/stretching exercises.
- Avoid squatting, sitting on floor as getting up can affect knee joints. Minimise sitting cross-legged or sitting in loose-legged position for long.
— The writer is chairman, Orthopaedics, Paras Hospital, Panchkula